|
Weight loss surgery does not cure diabetes or even remit it in
most cases on the long term and the risks far outweigh the benefits
especially after 10 years.
Thus I am rather shocked that in their
press release, the American Diabetes Assn recommends bariatric (weight
loss) surgery
for the treatment of diabetes.
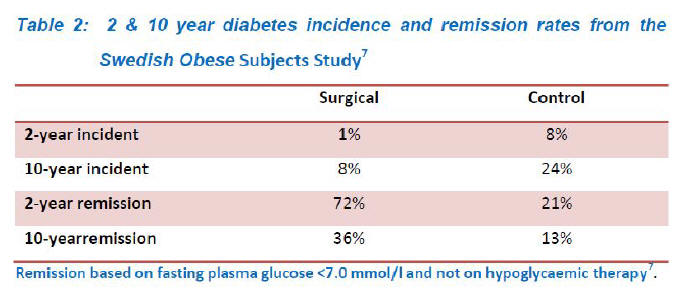
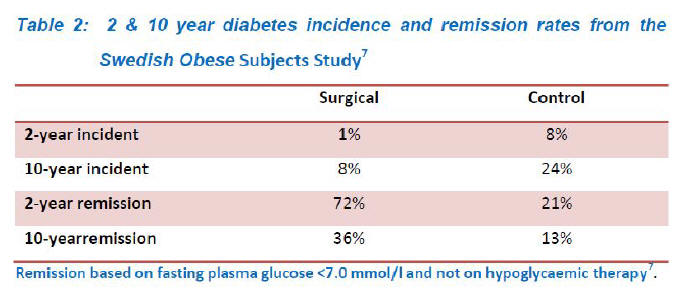
It's not surprising that they cited the Monash and Utah studies which
found at the two year post op point that 70-90 percent of diabetes were in
remission after weight loss surgery. However I am rather surprised
that they also cited the Swedish Obesity study which found at the 10 year
post op check that only 36% of diabetics remained in remission. How
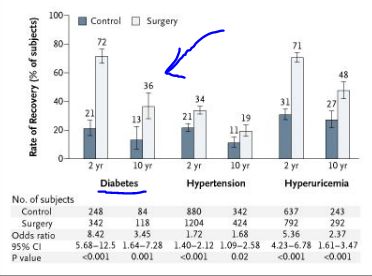
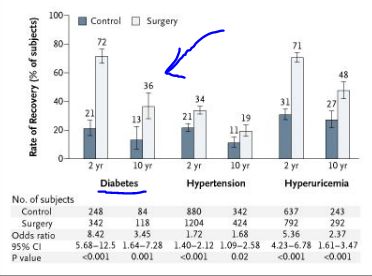
they got around that poor result is by producing the following chart
comparing those who had had weight loss surgery with those who had had no
intervention at all:
The above chart can be found on page 14 of the PDF entitled
"Bariatric Surgical and Procedural Interventions in the Treatment of Obese
Patients with Type 2 Diabetes"
One of the most telling studies was done in 2010. Researchers not only examined and followed a gastric bypass patient who claimed a cure for diabetes but also looked at 621 studies often cited to suggest weight loss surgery as a treatment for diabetes. They found that although the 55 year old patient claiming a cure, had a normal fasting blood sugar level and A1C of 6.x, he also had frequent blood sugar levels of 180 or more. And these same researchers found flaws in the 621 studies cited by weight loss surgery surgeons like Buchwald. They said most of the studies were retrospective, single-armed, and made up of relatively young women. Also, only 1.6% of them provided Class I evidence.
The study was presented at the American Association of Clinical Endocrinologists meeting, by two physicians, Anna Marina, MD, and Dace Trence, MD, of the University of Washington in Seattle. (Primary source: American Association of Clinical Endocrinologists - Source reference: Marina AL, Trence DL "Is diabetes mellitus really cured by gastric bypass surgery?" AACE 2010; Abstract 210. )
"Fasting blood glucose and HbA1c are insufficient criteria to establish remission of diabetes after surgery," Marina said. "Glucose tolerance tests or continuous glucose monitoring should be considered to provide a better assessment of glycemic status in this group of patients."
The researchers commented that these results were consistant with the Roslin study where 38 patients (i.e. 80 percent of the cohort) were found to have "irratic blood sugar levels" after gastric bypass. (Primary source: American Society of Metabolic and Bariatric Surgery - Source reference: Roslin M, et al "Abnormal glucose tolerance testing following gastric bypass" Surg Obesity Related Dis 2009; 5(3 Suppl): Abstract PL-205.)
Medical treatments have greatly improved with medications like
Metformin,
and also the information that even the safer procedures are fraught with complications is
easily accessible over the internet and certainly to medical providers and
the scientists connected with the ADA.
For example, the recent lap band
studies suggesting a high rate of complications equal with the gastric
bypass, with that procedure. There were several studies recently - here is
one in
Archives of Surgery (AMA) This study and others suggested that
the lap band, while considered much less invasive than the gastric
bypass because there is no dissection or bypassing of the small bowel or
any of the stomach as is true in the gastric bypass, caused 40% of patients to have complications requiring surgery.
(eroded band, slipped band, perforation of or damage to, the stomach,
inability to swallow etc)
Following is an article I sent to the editors of "Diabetes Forecast Magazine"
upon
their request in 2010 - including the research cites:
Although there has been a lot in the media lately
about diabetes and weight loss surgery, if one looks up the couple of studies that the claim
(that gastric bypass "cures" diabetes) is based on, the first thing
one finds is that none of the researchers ever used the word "cure"
- they used the word "remission" instead.
The study which has inspired a lot of media coverage (and
unfortunately, suggestions that people of normal weight who have
diabetes get a gastric bypass) was what we call "The Monash Study".
This study researched gastric bypass patients 2 years post op and
found that 72 percent of them with diabetes had gone into remission.
And that does sound impressive and actually the Swedish Obesity
Study, also found that result at the two year post op point i.e. 72
percent of diabetics had gone into remission.
However, the Swedish Obesity study also did a 10 year post op
follow-up and then, found that only 36 percent of the diabetics were
still "disease -free".
Cite: New England Journal of Medicine: Volume 351:2683-2693 December
23, 2004 Number 26 Lifestyle, Diabetes, and Cardiovascular Risk
Factors 10 Years after Bariatric Surgery Lars Sjostrom, M.D., Ph.D
et al
(chart showing these results)
This can be found among the charts in the article on:
http://www.nejm.org/doi/full/10.1056/NEJMoa035622#t=articleResults
Neither the Monash study nor the Swedish Obesity study were
"randomized".
cite: Monash study:
http://jama.ama-assn.org/cgi/content/full/299/3/316
A couple of things to keep in mind.
First of all, there is NO WAY, wrote one researcher to distinguish
whether early results of lowered sugar levels from a gastric bypass,
are actually due to the surgery or rather due to the fasting
patients are doing right after surgery:
For instance, since patients undergoing Roux-en-Y gastric bypass
(RYGB) or biliopancreatic diversion (BPD) eat small, rather fluid
and low-caloric meals in the early postoperative period, it is
admittedly impracticable to rule out that the rapid normalization of
plasma glucose and improved insulin resistance after these surgeries
be simply the effect of decreased caloric intake. [Effect
of Duodenal-Jejunal Exclusion in a Non-Obese Animal Model of Type 2
Diabetes: A New Perspective for an Old Disease Francesco Rubino, MD
and Jacques Marescaux, MD, FRCS University Louis Pasteur,
Strasbourg, France]
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1356426/
Secondly,
no study has been designed to see if the risks of the surgery
outweigh the benefits, as one blogger researcher has written:
http://junkfoodscience.blogspot.com/2009/01/bariatric-surgery-for-diabetic-teens-in.html
Third, it should be kept in mind that early diabetes is extremely
responsive to lifestyle changes alone (diet and exercise) but even
later term diabetes can be kept well under control with reasonably
safe medications like Metformin especially if combined with minor
lifestyle changes. Modern testing equipment tests blood sugar levels
rather accurately, and is easily done by patients. Thus the
dour predictions about diabetes given in the 1960's before modern
treatments and advanced knowledge about diet and exercise, are
likely no longer valid.
An analysis of the Monash (and Swedish Obesity) studies and diabetes
can be found at the following:
http://suethsayings.blogspot.com/2009/02/re-visit-diabetes-and-weight-loss.html
Do the risks of bariatric surgery outweigh the
benefits?
Unfortunately, we still, to date, have no studies to confirm or deny
this however, the following are medical opinions which question
this:
Dr Edward Mason who invented the gastric bypass, did so in 1965
after observing that his "Billroth II" patients (surgery to correct
a duodenal ulcer - this is done with medication now) had a difficult
time keeping their weight in the so called "normal" range (they were
fighting to avoid being underweight) and so he opined that doing a
similar surgery on very obese people would help them to be slimmer.
But by the time he had done this surgery (gastric bypass) on people
for 15 years and did the follow-up, he concluded that the amount of
complications due to vitamin malabsorption and other complications
outweighed any benefits of the surgery. He wrote:
"For the vast majority of patients today, there is no operation
that will control weight to a "normal" level without introducing
risks and side effects that over a lifetime may raise questions
about its use for surgical treatment of obesity."
http://obesitysurgery-info.com/masonpromvgb.htm
And he invented another surgery which called for stapling the
stomach ONLY but not bypassing any stomach or small bowel called the
"Vertical Banded Gastroplasty" which he began advocating rather than
the gastric bypass (which HE himself had invented!). In the years
following, he wrote a lot about how perhaps the gastric bypass
wasn't the best idea because we were learning more and more about
the stomach.. for example:
" The future of weight loss surgery rests in greater use of
simple stomach restriction procedures like vertical banded
gastroplasty, which preserve the normal weight-maintenance
mechanisms of the body," Mason said. "If simple restriction
procedures did not produce sufficient weight loss, it was always my
inclination to work with the patient to solve other problems
affecting weight loss rather than going to a more radical
procedure."
http://obesitysurgery-info.com/mason-u-of-i-article-2003.htm
When considering bariatric surgery for diabetes especially gastric
bypass, a clinical study by Roslin et al should be taken in
consideration:
The researchers also found that 80 percent of the patients also
had undiagnosed "glucose abnormalities" including "high blood sugar"
or "low blood sugar" or both. Dr. Roslin reported on this study at
the 2009 ASMBS convention, suggesting that the gastric bypass may
cause a heightened insulin response due to the rapid emptying of the
pouch into the small bowel.
Roslin M, et al "Abnormal glucose tolerance testing following
gastric bypass" Surg Obesity Related Dis 2009; 5(3 Suppl): Abstract
PL-205.
http://www.medpagetoday.com/MeetingCoverage/ASMBS/14874
That is, in this case, the cure may be far worse than the disease
(diabetes) because it so far, has alluded providers as to how to
treat "reactive hypoglycemia" from gastric bypass which can cause a
plethora of highly disabling symptoms including seizures and passing
out from extremely low blood sugar levels. This condition is thought
to be caused by the death of the pancreatic "islet" cells (as a
repercussion of the surgery) and is apparently far more common than
previously thought, in gastric bypass patients.
Two patients who are suffering with reactive hypoglycemia:
Beth Sheldon-Badorre who complains about how blood sugar levels
can totally bottom out (like 30 or lower) with no notice, for
example while she is driving:
http://tinyurl.com/hypoglycemia-driving
Another blog about this complication in a gastric bypass patient:
http://bariatriceating.com/SMblog/?p=366
As Dr Livingston, a bariatric surgeon himself has written:
***** "By doing this surgery, you're creating a medical disease in
the body. Before you expose someone to that risk, you have to be
absolutely sure that you are treating an illness which is equal to
or greater than the one you are creating."
(Dr Edward Livingston, bariatric surgeon in Self Magazine, 4-2001)
*****
And even the American Medical Association has never guaranteed any
results with this surgery - they commented that although early
results were impressive, long term results (and complications) were
basically "unresolved":
****" Short-term outcomes are impressive-patients undergoing
bariatric surgery maintain more weight loss compared with diet and
exercise. Comorbidities such as type 2 diabetes can be reversed. But
long-term consequences remain uncertain. Issues such as whether
weight loss is maintained and the long-term effects of altering
nutrient absorption remain unresolved."****
In the same comment, they warned their members to "avoid the ethical
haze" associated with bariatric surgery:
**** The ethical haze surrounding bariatric procedures is not
unknown in surgery, said Laurence B. McCullough, PhD, a professor of
medicine and medical ethics at Baylor College of Medicine in
Houston, Texas.
"This is the classic problem in surgery-innovation without the
research to guide it. So all this should be brought under
experimental protocols," McCullough said. "That's how you handle the
conflict of interest make sure you tell the patient, 'The procedure
is investigational; we don't know if it will help you."' ****
1762 JAMA, April 9, 2003-VoL 289, No. 14
For those who think the new vertical sleeve gastroplasty might be
the answer, here is the website of a gastroplasty patient who had
that surgery (merely stapling across the stomach - i.e. not the VSG
which calls for the removal of 90 percent of the stomach which is
taken out of the body and sent to pathology) 30 years ago.
The following website is of a 30 year post op patient with an
"in-tact" gastroplasty (bariatric surgery) who has brittle diabetes
- type II (among many other problems):
http://ozobesitysurgery-info.webstarts.com/
Vicki at the above site described being rather ill from her
gastroplasty including having brittle diabetes. She is
deceased - died from choking in 2010.
Hope this has been useful to you. Please feel welcome to write me
for further information and/or aid.
|
I would sincerely hope the American Diabetes Assn and medical providers
treating diabetes would search the internet and consider carefully, the
risks and benefits before suggesting weight loss surgery to treat diabetes
(which seems unnecessary as medical treatment thereof has progressed so
much in the last decade.
|